
PERSERIS® is indicated for the
treatment of schizophrenia in adults.
Downloadable
resources
PERSERIS Clinical Resource for HCPs

PERSERIS Clinical Resource for HCPs
A resource for key clinical information about PERSERIS including pharmacokinetics, efficacy, and safety. Download as a reference for yourself or share with a colleague.
PERSERIS Injection Resource for HCPs
A guide to getting started with PERSERIS, including information about straightforward initiation, how to administer, the depot delivery system, and clinical data of injection site pain & reactions. Download as a reference for yourself or share with a colleague.
PERSERIS Injection Resource for HCPs
PERSERIS Guide for Patients
PERSERIS Guide for Patients
Download or email and share with your patient and/or their support system to help them learn more about PERSERIS, including what to expect at their appointments, and how PERSERIS treatment may help manage their schizophrenia.
HCP=healthcare provider.
Identifying Patients
Once-Monthly Dosing
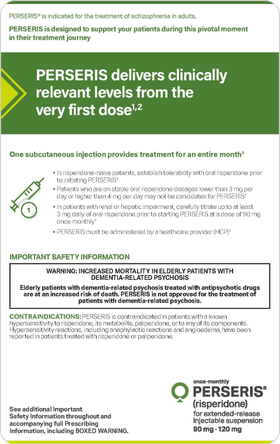
IMPORTANT SAFETY INFORMATION
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. PERSERIS is not approved for the treatment of patients with dementia-related psychosis.
CONTRAINDICATIONS: PERSERIS is contraindicated in patients with a known hypersensitivity to risperidone, its metabolite, paliperidone, or to any of its components. Hypersensitivity reactions, including anaphylactic reactions and angioedema, have been reported in patients treated with risperidone or paliperidone.
WARNINGS AND PRECAUTIONS
Cerebrovascular Adverse Reactions: In trials of elderly patients with dementia-related psychosis, there was a significantly higher incidence of cerebrovascular adverse reactions (e.g., stroke, transient ischemic attack), including fatalities, in patients treated with oral risperidone compared to placebo. PERSERIS is not approved for use in patients with dementia-related psychosis.
Neuroleptic Malignant Syndrome (NMS), a potentially fatal symptom complex, has been reported with antipsychotic medications. Clinical manifestations include hyperpyrexia, muscle rigidity, altered mental status including delirium, and autonomic instability (see full Prescribing Information). Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure. If NMS is suspected, immediately discontinue PERSERIS and provide symptomatic treatment and monitoring.
Tardive Dyskinesia (TD) may develop in patients treated with antipsychotic drugs. The risk of developing TD and likelihood that it will become irreversible are believed to increase with treatment duration and total cumulative dose. TD can develop after relatively brief treatment periods even at low doses, or after treatment discontinuation. Elderly patients, especially elderly women, appear to be at increased risk, but it is impossible to predict which patients will develop TD. Therefore, PERSERIS should be prescribed in a manner that is most likely to minimize the occurrence of TD. Discontinue treatment if clinically appropriate.
Metabolic Changes that may increase cardiovascular/cerebrovascular risk, have been associated with atypical antipsychotics (APs).
- Hyperglycemia and Diabetes Mellitus (DM), in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, have been reported in patients treated with APs, including risperidone. Patients with DM who are started on atypical APs, including PERSERIS, should be monitored regularly for worsening of glucose control. Patients at risk for DM (e.g., obesity, family history of diabetes) who are starting treatment with atypical APs, including PERSERIS, should undergo fasting blood glucose (FBG) testing at the beginning of treatment and periodically while treated. Any patient treated with atypical APs, including PERSERIS, should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical APs, including PERSERIS, should undergo FBG testing. In some cases, hyperglycemia has resolved when risperidone was discontinued; however, some patients required continuation of antidiabetic treatment despite discontinuation of risperidone.
- Dyslipidemia has been observed in patients treated with atypical APs. When initiating PERSERIS, obtain a fasting lipid profile and monitor periodically during treatment.
- Weight Gain has been observed with atypical AP use. Monitoring weight is recommended.
Hyperprolactinemia: Risperidone elevates prolactin levels, and the elevation persists during chronic administration. Risperidone is associated with higher levels of prolactin elevation than other antipsychotic agents. Hyperprolactinemia may inhibit reproductive function in female and male patients. Galactorrhea, amenorrhea, gynecomastia, and impotence have been reported in patients receiving prolactin-elevating drugs. Long-standing hyperprolactinemia, when associated with hypogonadism, may lead to decreased bone density in females and males.
Orthostatic Hypotension and Syncope: Risperidone may induce orthostatic hypotension associated with dizziness, tachycardia, and in some patients, syncope, particularly at treatment initiation, re-initiation, or dose increase. Use with particular caution in patients with known cardiovascular disease, cerebrovascular disease, and conditions which predispose patients to hypotension, and in the elderly and patients with renal or hepatic impairment. Monitor such patients and consider a dose reduction if hypotension occurs.
Falls: Somnolence, postural hypotension, motor instability, and sensory instability have been reported with the use of antipsychotics, including PERSERIS, which may lead to falls, and consequently, fractures or other fall-related injuries. Assess the risk of falls when initiating treatment and recurrently during treatment.
Leukopenia, Neutropenia, and Agranulocytosis have been reported with antipsychotic agents, including risperidone. In patients with history of clinically significant low white blood count (WBC) or absolute neutrophil count (ANC), or history of drug-induced leukopenia or neutropenia, perform a complete blood count frequently during the first few months of therapy. Consider discontinuation at the first sign of clinically significant decline in WBC in the absence of other causative factors. Monitor patients with clinically significant neutropenia for fever or other symptoms/signs of infection; treat promptly if such symptoms/signs occur. Discontinue PERSERIS in patients with ANC <1000/mm3 and follow WBC until recovery.
Potential for Cognitive and Motor Impairment: Antipsychotics including PERSERIS may cause somnolence and impair judgment, thinking, and motor skills. Caution patients about operating machinery, including motor vehicles, until they are reasonably certain PERSERIS does not affect them adversely.
Seizures were observed in risperidone studies in adults with schizophrenia. PERSERIS should be used cautiously in patients with a history of seizures or other conditions that potentially lower the seizure threshold.
Dysphagia: Esophageal dysmotility and aspiration can occur. Use cautiously in patients at risk for aspiration.
Priapism has been reported with other risperidone products. Severe priapism may require surgical intervention.
Body Temperature Regulation: Atypical antipsychotics may disrupt the body’s ability to reduce core body temperature. Use with caution during strenuous exercise, exposure to extreme heat, dehydration, or when taking anticholinergic medications.
ADVERSE REACTIONS: The most common adverse reactions in a clinical trial (≥ 5% and greater than placebo) were increased weight, constipation, sedation/somnolence, pain in extremity, back pain, akathisia, anxiety, and musculoskeletal pain. The most common injection site reactions (≥ 5%) were injection site pain and erythema. This is not a complete list of potential adverse events. Please see the full Prescribing Information for a complete list.
DRUG INTERACTIONS
- Carbamazepine and other strong CYP3A4 inducers decrease risperidone plasma concentration.
- Fluoxetine, paroxetine, and other strong CYP2D6 inhibitors increase risperidone plasma concentration.
- Use with other CNS drugs or alcohol may increase nervous system disorders.
- PERSERIS may enhance hypotensive effects of hypotensive agents.
- PERSERIS may antagonize the pharmacologic effects of dopamine agonists.
- Dosage change in PERSERIS or methylphenidate may increase risk of extrapyramidal symptoms.
USE IN SPECIFIC POPULATIONS
Pregnancy: PERSERIS may cause extrapyramidal and/or withdrawal symptoms in neonates with third trimester exposure. Advise patients to notify their healthcare professional if they become or intend to become pregnant during treatment with PERSERIS. Patients exposed to PERSERIS during pregnancy may be registered with the National Pregnancy Registry for Atypical Antipsychotics (1-866-961-2388 or http://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/).
Lactation: Infants exposed to risperidone through breastmilk should be monitored for excess sedation, failure to thrive, jitteriness, and extrapyramidal symptoms.
Pediatric Use: Safety and effectiveness of PERSERIS have not been established in pediatric patients.
Renal or Hepatic Impairment: Carefully titrate on oral risperidone up to at least 3 mg before initiating treatment with PERSERIS at a dose of 90 mg.
Patients with Parkinson’s Disease or dementia with Lewy Bodies can experience increased sensitivity to risperidone. Manifestations can include confusion, obtundation, postural instability with frequent falls, extrapyramidal symptoms, and clinical features consistent with NMS.
To report a pregnancy or side effects associated with taking PERSERIS or any safety related information, product complaint, request for medical information, or product query, please contact PatientSafetyNA@indivior.com or 1-877-782-6966.
P-RAG-US-00649